Only vaccines or drugs will end social distancing
Governments around the world are exploring how to exit lockdowns that suppress COVID-19 without a resurgence
The United Kingdom last week launched a nationwide surveillance study to track how many people have been infected with SARS-CoV-2, the virus that causes COVID-19. Studies currently estimate that only a small fraction of people were infected prior to strict social-distancing enforcement. A major second wave of COVID-19 cases and deaths is likely if countries exit lockdowns without strategies to reduce transmissibility of the virus. However, policymakers have few tried-and-tested strategies to fall upon as the situation is unprecedented. Researchers are now rushing to produce models to estimate the impact of epidemic mitigation strategies while they wait for more data.
What next
Contact tracing and isolation in addition to some form of social distancing will be needed for months in order to avoid overwhelming hospitals' intensive care capacities -- until a vaccine or levels of population infection help build 'herd immunity' or pharmaceutical interventions reduce mortality rates. Social distancing of the most vulnerable will likely continue until an effective vaccine is available.
Subsidiary Impacts
- A new London School of Hygiene and Tropical Medicine platform, pooling worldwide interventions, could help clarify intervention effects.
- Long-term social distancing will particularly harm the wellbeing of the unemployed, self-employed and elderly in particular.
- Continued remote working or cyclical return to work will help moderate demand on healthcare capacity in the medium term.
- International travel restrictions will have a lasting impact on the travel and tourism sectors.
Analysis
Lockdowns have been a stringent course of action to mitigate the mortality resulting from COVID-19 and to protect healthcare services from collapse. Such measures are unprecedented, and their effectiveness is only just beginning to be studied. Furthermore, the pandemic is still in early stages and there are key unknowns, for example, how many people have been infected with SARS-CoV-2.
Virus prevalence
The most comprehensive general population screening for virus infection, conducted in Iceland, yielded virus prevalence estimates of less than 1% based on two time points.
Serological surveys assessing population exposure to SARS-CoV-2, based on cumulative rather than current infections are lacking. Various surveys attempting to capture a random sample of the population conducted in Germany, the Netherlands and United States have estimated population exposures, capturing all infections that have occurred in those populations to date, ranging from 2% to 30%. Modelled estimates for Europe suggest that only a small fraction of populations were likely infected prior to lockdown, from a low of 0.4% in Norway to a high of 15% in Spain.
Surveys and estimates of the virus's prevalence range from 2% to 30%
The upper limit of these estimates is considered insufficient to achieve 'herd immunity', a concept whereby a sufficient level of population immunity disrupts the spread of infection, by providing indirect protection to those without immunity. Herd immunity requirement is highly pathogen- and setting-specific, but based on epidemiological theory, over 60% population immunity is required to halt the growth of the epidemic in most countries, depending on the estimated 'effective reproduction number' (average number of secondary cases per infected individual).
This suggests that a second large waves of infection and deaths will likely ensue if lockdown measures are lifted without effective mitigating measures in place.
Baseline scenario
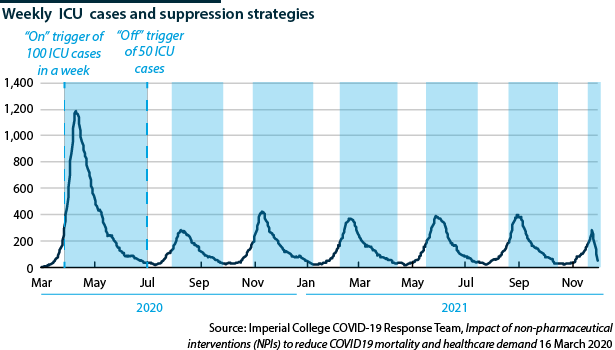
As the effects of mitigating measures are being studied for their effectiveness, policymakers are currently relying on models and modelled scenarios. The baseline scenario to control the epidemic involves alternating relaxing and tightening strict social distancing measures.
Modelling studies from the United States and United Kingdom estimate that without medical or technological interventions such as a vaccine, these measures will be needed to avoid exceeding critical care bed capacity until countries reach herd immunity.
The US study estimates that the virus may be in circulation in the United States until 2022 and could resurge in 2024 even if supressed -- though variables such as seasonal variation, immunity and intensity of social distancing would change this timeline (see INTERNATIONAL: Social distancing will last for months - March 18, 2020 and see INTERNATIONAL: Virus tests may not lift lockdowns soon - April 3, 2020).
These 'adaptive trigger' approaches require effective population or hospital-based surveillance of infection -- necessitating a massive increase in testing capacity.
Lockdown exit scenarios
Researchers are exploring how to exit lockdowns.
A French study has modelled the impact of various measures in the Paris region, including school closures, the number of people working remotely, isolation of the elderly, banning social events and non-essential activities, and case isolation. They predict a second epidemic wave would ensue -- requiring 2.5 times the intensive care bed capacity -- even under stringent social distancing, including school closures and isolation of the elderly, unless rigorous case finding and isolation is also implemented. They note that case finding and isolation would need to be most efficient in the first month after lifting lockdowns to reduce the case load on hospitals during the second wave.
The role of children in the spread of COVID-19 is not established and so exit strategies relating to this group will vary between countries, with some choosing to reopen schools and others opting to delay. Countries that reopen schools early could provide some insight into what effect this option might have on the epidemic.
The University of Warwick Business School presents a 'release the young from lockdown' approach. Here, measures are relaxed on, for example, 20-30 year-olds not living with parents and could potentially involve a staged release of older adults who test antibody positive. This approach recognises the impact of social distancing measures on unemployment, future incomes and national debt, and would enable the economy to restart through the young workforce, providing support for society as a whole. However, they recognise that deaths would rise among this younger cohort. Case fatality rates for 20-30 year-olds vary from 0.06% to 0.15%, while estimates exceed 3.99% for 60-69 year-olds, 8.61% for 70-79 year-olds and 13.4% for over 80s, according to a Lancet study
An interesting conceptual model proposes a cyclical return to work that may allow for some return to economic activity while suppressing the epidemic. An Israeli modelling study investigates a pattern of four-days work, ten-days lockdown, allowing for part-time employment. This approach does necessitate the employment of other measures, such as hand washing, physical distancing and importantly it assumes rapid isolation of cases and contacts is maintained throughout.
Sweden has also offered a potentially attractive model on social distancing for the control of COVID-19. Their epidemic has not grown at the rate experienced by other European countries, despite their comparatively soft approach to mitigating, rather than suppressing, the spread of COVID-19. However, a modelling study, based on the framework of the UK's Imperial College COVID-19 Response Team, predicts Sweden may soon be on its way to exceeding its national intensive care capacity 40-fold if stricter social distancing measures are not rapidly enforced.
Testing and contact tracing
A consistent conclusion is that while prolonged social distancing could delay epidemic peaks and reduce peak incidence, intensive care hospital capacity is still likely to be exceeded in many countries in the absence of rigorous and fast testing capacity to identify and isolate infected people and their contacts ('test-trace-isolate'). These diagnostic tests identify the presence of virus in a nasal swab to confirm infection. This allows for cases to be isolated, as well as others they may have unknowingly exposed, as identified through contact tracing.
A recent study from the Imperial College COVID-19 Response Team, modelling the impact of virus testing on the control of the disease in the United Kingdom, suggests that mass-scale testing may not be a necessary part of an exit strategy. It concludes that testing is unlikely to limit the transmission of the virus more than existing policies of contact tracing and isolation on symptom onset given that testing currently is slow and not especially accurate.
A technological solution where an index case's contacts are immediately notified on symptom onset and then self-isolate would be more effective in controlling the epidemic provided there is high public participation (see INTERNATIONAL: Inaccuracy and speed dent virus testing - April 24, 2020). Nonetheless, testing is crucial in helping epidemiologists gain an accurate picture of the pandemic and allowing policymakers to form effective strategies to manage it.
Aggressive contact tracing is key in keeping the virus's transmissibility low
In some countries, the control of COVID-19 has witnessed the evolution of digital contact tracing technology via proximity sensors on mobile phones (see EUROPE: COVID-19 tracking tech will proliferate - April 15, 2020). There are concerns surrounding data protection and civil liberties owing to the transfer of personal information, and the potential abuse by law enforcers if personal data are held centrally and used for purposes other than managing the health crisis. However, South Korea has tried to mitigate this through publishing anonymised information, such as travel routes and public transport that infected people took. Some Western countries, notably Switzerland, are developing decentralised systems that involve anonymous submission of key data to preserve privacy.
In addition, the use of 'immunity passports' is being discussed as part of exit strategies. This approach relies on detection of antibodies in blood serum to identify people who have previously been exposed to the virus. Only once they reach threshold accuracy, these antibody tests may allow for some people to return to work as they may no longer be at risk of contracting and spreading the infection. Moreover, it is unlikely that these tests will be readily available for mass employment as part of exit strategies in the near future.
Testing problems
At present, neither diagnostic nor antibody tests correctly classify a person as positive or negative 100% of the time. In the case of COVID-19, there are limited validations available for antibody tests and those suggest 67% to 95% cases may correctly test positive (test sensitivity), while around 74% to 98% of negative individuals may correctly test negative (test specificity). Most human tests applied in the routine healthcare setting have a sensitivity and specificity over 95%.
One modelling study suggests a sensitivity of around 85% would be sufficient for virus detection tests to have a beneficial impact on the control of disease at the population scale, even if the false negative rate is high. However, this is in the unlikely scenario that the entire population was regularly tested.
Immunity unknowns
Moreover, the detection of antibodies does not yet confirm someone is protected from future infection -- the virus will almost certainly confer antibody protection, but not all antibodies give rise to antiviral activity that protects against reinfection. The types of antibodies needed are known as 'neutralising' antibodies.
Key uncertainties remain around immunity to the virus
At the moment, little is known about whether neutralising antibodies are generated by COVID-19 infection, and it is not known whether all antibody tests detect these protective kinds of antibody. A recent antibody test development from the United States shows promising results that COVID-19 infection likely generates antibodies that can protect against reinfection. Studies are now urgently needed to determine how levels of antibody in the blood correlate with the likelihood, degree and length of protection.
Logistical bottlenecks
The application of virus testing as part of exit strategies will depend on the ability for mass testing. This has not been achieved in most countries and there is now a global bottleneck in commercial laboratory supplies.
In the case of immunity passports, because antibody tests require careful validation, they cannot be rapidly developed for mass rollout in the context of a newly discovered virus and are unlikely to feature in exit strategies in the near term. One key problem is access to positive sera to develop antibody tests -- patients must have recovered for around four weeks before their blood is useful for test development and some labs have been waiting for weeks to get samples.
Outlook
Some form of social distancing will need to continue until an effective vaccine and/or drugs are available for mass use in order to preserve the functioning of critical care hospital facilities.
The deployment of vaccines and antivirals will vary across countries depending on the scientific demonstration of efficacy and safety by robust clinical trials, the attractiveness of either or both developments to manufacturers, and the control by regulatory authorities. The extent of social distancing interventions needed will also vary depending on the capacity for virus testing, to identify and isolate cases and their contacts.