Cross-immunity would aid COVID-19 battle
Scientists are studying whether seasonal 'common cold' viruses confer some immunity against COVID-19
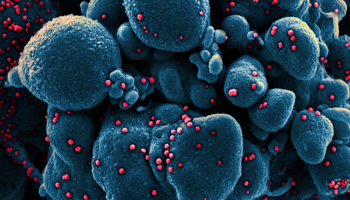
The severity of COVID-19 effects differs between individuals. This is partly attributed to age and to health predispositions, but the physiological basis is not entirely clear. Existing immunity from previous exposure to other coronaviruses -- or cross-immunity -- may affect how individuals respond to SARS-CoV-2 infection. Studies are investigating whether past exposure to different but related viruses make people more or less susceptible to a new form, but there are no definitive answers yet.
What next
With time, more information may allow cross-immunity to be viewed as a risk or protective factor. Cross-immunity may play some protective role against SARS-CoV-2 infection and the development of severe COVID-19 in certain populations, but this may not be a clear defining factor that can be used to predict risk and outcome in the current phase of the pandemic. Understanding why some people are more susceptible to severe disease will be important in guiding further policy and behaviour and identifying better pharmaceutical interventions.
Subsidiary Impacts
- Governments and scientific advisers may be able to use cross-immunity to identify the most at-risk groups in this and future outbreaks.
- Cross-immunity may affect policy on schools and age-based institutions during the COVID-19 pandemic.
- Vaccine and drug developers will benefit from understanding cross-immunity to refine pharmaceutical development.
Analysis
Immunity is defined as a protective state against infection and disease caused by pathogens such as viruses (see INTERNATIONAL: Immunity will shape pandemic's future - June 26, 2020). This involves antibodies and immune cells, which can recognise parts of proteins from infective agents.
Cross-immunity is broadly defined as a situation where an immune response to one infection confers protection against another, distinct infection or disease. This happens when adaptive immune components such as antibodies recognise different pathogens because of structural similarities. This is called 'cross-reactivity'.
Cross-reactivity is not always protective. In some certain cases, existing immune responses can promote disease or enhance its severity.
Both kinds of effects -- protection and exacerbation -- may be relevant to SARS-CoV-2. The outcomes of SARS-CoV-2 infection are variable: some individuals are asymptomatic or show mild symptoms, while others progress to hospitalisation, life-support or death.
Cross-reactivity?
There are few well-understood examples of cross-reactivity between viruses.
Influenza is a example of protective effects: one strain can confer protective antibody responses to other strains.
The dengue virus exemplifies the reverse effect: a first infection with one type typically leads to mild illness, but subsequent infection with a distinct serotype is associated with lethal disease, through a process known as antibody-dependent enhancement.
Coronavirus family
Coronaviruses are highly diverse and widespread and infect many animal species. The different types of coronavirus share similarities of structure and proteins.
Of the seven known coronaviruses that infect humans, four are endemic and seasonal and are referred to as 'common cold' coronaviruses (229E, NL63, HKU1 and OC43). The others are the emerging SARS-CoV-1, SARS-CoV-2 and MERS-CoV.
SARS-CoV-1 is presumed extinct shortly after its emergence in 2002-03. MERS-CoV is endemic in camels and typically jumps to humans, causing disease in a few thousand people per year, primarily in the Middle East.
SARS-CoV-2, the virus of the current pandemic, is related more closely to the beta coronaviruses (SARS-CoV-1, MERS, HKU1 and OC43) than to the alpha coronaviruses (NL63 and 229E), the other lineage of the Coronaviridae family. Both lineages contain viruses that infect other species such as bats.
Infection with the endemic group of coronaviruses is frequent and believed to be more prevalent in children and young adults than in the older population. A recent study of pre-pandemic samples from the UK population showed that 60% of individuals aged 6-16 years had antibodies that could recognise SARS-CoV-2. This was lower among older people.
Evidence of cross-immunity for COVID-19 is not yet conclusive
Other studies have shown that although communities do harbour antibodies that cross-react with SARS-CoV-2, these antibodies do not necessarily offer protection from COVID-19. Any immunity to SARS-CoV-2 conferred by such antibodies is expected to be short-lived, so an individual could be repeatedly infected.
There remains a concern around antibody-dependent enhancement (as in the dengue example). This is known to have occurred in certain cases with regard to SARS-CoV-1. There is no evidence yet that this is affecting vaccine development for COVID-19.
An elevated immune response to first infection could prevent re-infection
Studies in animals have shown that immunity from first infection protects against re-infection, at least for a short duration -- the length of the experiment, at least a few weeks. Also, vaccines that induce SARS-CoV-2 antibodies and T-cells are protective against lung infection and subsequent disease.
One study from September 2020 identified a protective effect against COVID-19 conferred by recent endemic coronavirus infection, but this effect was only minor.
There have been a few cases of natural re-infection in humans, indicating that it is possible. One determinant may be the level of immunity created by first exposure. A more severe infection will raise higher levels of antibodies, so could prove to have a better subsequent protective effect than that in people who were asymptomatic first time.
Implications of cross-immunity
If cross-protective immunity exists , this could help explain the variability in COVID-19 severity between individuals, and simple tests could predict possible outcomes. It could also pave the way for a safe and effective SARS-CoV-2 vaccine in the form of immunisation with seasonal coronaviruses, which are well-studied and well-tolerated in most populations (see INT: COVID vaccine roll-out will face multiple hurdles - October 14, 2020).
If seasonal coronaviruses protect against COVID-19, they could be used in vaccines
Similarly, this could also have an effect if SARS-related coronaviruses become pandemics in the future. In a future SARS-CoV outbreak, the human population could be somewhat protected against it.
If cross-reactivity were found not to be protective against infection and disease, this would mean that other reasons lie behind the variability in responses. Discerning these would be extremely important for the long-term management of COVID-19.
In a worst-case scenario, where cross-reactivity does exist but its effect is to promote severe COVID-19, antibody-dependent enhancement could complicate vaccination as well as infection management in future. No evidence to support this has been identified so far, but it remains a possibility, perhaps applying to some individuals.